What is peritoneal dialysis?
Abdominal cavity is lined by peritoneal membrane which acts as a semi- permeable membrane to effect diffusion of solutes (toxic substances of metabolism e.g. urea, creatinine and others) and removal of excess water (ultrafiltration) from blood into the dialysate contained in the abdominal cavity.

(Fig. 9.a) principles of dialysis - diffusion for solutes removal ie waste products of metabolism
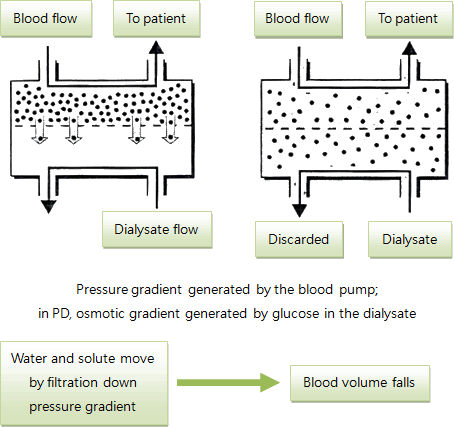
(Fig. 9.b) principles of dialysis - convection (ultrafiltration) mainly for water removal (also solutes dissolved in water)
Dialysate is a type of glucose solution with variable concentration (higher concentration has higher osmolarity and so faster ultrafiltration) which is higher than blood so that excess fluid in the body is removed into abdominal cavity through the process of ultrafiltration down the osmotic gradient generated by the glucose solution which is installed into the cavity through a pre-inserted tubing (catheter).
A tubing (catheter) is inserted by surgical operation into peritoneal cavity to allow the draining in and out of dialysate into the abdominal cavity.
A cycle of peritoneal dialysis consists of draining in of dialysate, dwelling of dialysate in the abdominal cavity (time for dialysate to be in contact with the peritoneal membrane) and the draining out of dialysate when the cycle is completed.

(Fig. 10) one cycle of peritoneal dialysis:
- draining in of dialysate from dialysate bag;
- dwelling of dialysate in the abdominal cavity (time for diffusion and convection);
- draining out of dialysate from the abdomen.
Peritoneal dialysis (PD) can carried out in the daytime 3-4 cycles manually named continuous ambulatory PD (CAPD) or while sleep at night 4-6 cycles or more automatically by a computer programmed cycler named automatic PD (APD).
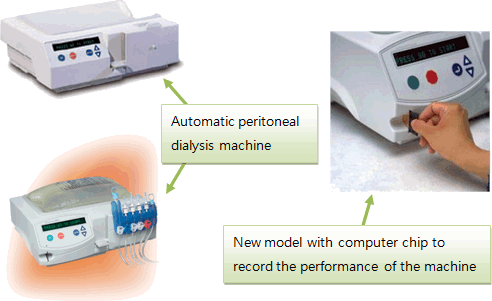
(Fig. 11.a) automatic cycler machine (computerized)

(Fig. 11.b) a child on APD while sleeping
APD is the preferred mode for it gives more freedom to the child in the daytime to go back to school and participate in other social activities; and also more time for the caretaker to pursue their own activities.
There are pre-requisites to carry out peritoneal dialysis:
- The child should have a normal or near normal peritoneal cavity which can be damaged due to previous abdominal surgery or peritonitis (infection of the peritoneal membrane)
- The presence of a trainable caretaker at home to carry out the procedure. An adolescent can also carry out the procedure by oneself.
- Home environment is spacious enough to store bags of dialysate solution and other equipments such as tubings, stainless steel trolley.
- The caretaker has to undergo a training program and get a pass after being assessed by the nursing paediatric renal specialist (P5 Paediatric Nephrology ward of Princess Margaret Hospital).
Major problems with peritoneal dialysis are peritonitis and exit site infection (ESI):
- Peritonitis is the inflammation of the peritoneal membrane secondary to bacterial infection (occasionally fungal or others); and it presents with abdominal pain, cloudy effluent dialysate and fever. Prompt treatment is necessary to preserve membrane function.
- ESI is the infection at the site where the tubing is inserted through the skin. It is also usually caused by bacteria and presents with pain, swelling and redness and discharge purulent at the site.
- As infection is so important, meticulous attention is needed in the aseptic technique in carrying the procedure of peritoneal dialysis at home.
- Sometimes catheter may have malfunction (usually poor outflow) as a result of blockade or migration to other part of the abdomen.
- Home
- About Us
- Kidney Health
- What are the causes of kidney disease in children?
- How to keep kidneys healthy?
- Do you have kidney problem?
- Chronic Renal Failure (CRF) & Renal Replacement Therapy (RRF)
- What is peritoneal dialysis?
- What is hemodialysis?
- What is kidney (renal) transplantation?
- FAQs for CRF and renal replacement therapy
- Services
- Sharings
- Support Us
- Contact
- Introductory information and Photos of Activities
- Online Donation Form
- Related Links

